Colonoscopy
Colonoscopy is a test to view the inside of your lower digestive tract (colon and rectum). Sometimes it can show the last part of the small intestine (ileum). During the test, small pieces of tissue may be removed for testing. This is called a biopsy. Small growths, such as polyps, may be removed.
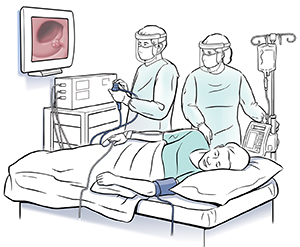 |
| A camera attached to a flexible tube with a viewing lens is used to take video pictures. |
Why is colonoscopy done?
The test is done:
-
To look for colon cancer or polyps
-
To help find the source of belly (abdominal) pain or bleeding
-
To help find the cause of changes in bowel habits
It may be needed every 5 to 10 years. Or it may be needed more often. This depends on factors, such as your:
Risks and possible complications
These include:
-
Bleeding
-
A hole (puncture) or tear in the colon
-
Risks or reaction to sedation medicine (anesthesia)
-
A cancer sore (lesion) not being seen or fully removed from past testing or procedures
Getting ready
To prepare for the test:
-
Talk with your healthcare provider about the risks of the test (see below). You can also ask about other options.
-
Tell your provider what medicines you take. This includes over-the-counter and prescription medicines. It also includes vitamins, herbs, and supplements. You will likely be advised to stop taking any blood-thinning medicines before the test.
-
Tell your provider what health conditions and allergies you have.
-
Make sure your rectum and colon are empty for the test. This is done by following the diet and bowel prep instructions exactly. If you don’t follow the directions, the test may need to be rescheduled.
During the test
The test is often done in the hospital on an outpatient basis. Or it's done at an outpatient clinic. Outpatient means you go home the same day. The procedure usually takes about 30 minutes. During that time:
-
You're given relaxing (sedating) medicine through an IV (intravenous) line. You may be drowsy. Or you may fall asleep.
-
The healthcare provider will first give you a physical exam. This is done to check for anal and rectal problems.
-
Then the anus is lubricated and the scope is inserted.
-
You may feel like you need to have a bowel movement if you're awake. You may feel pressure as air is pumped into the colon. It’s OK to pass gas during the procedure.
-
Biopsy, polyp removal, or other treatments may be done during the test.
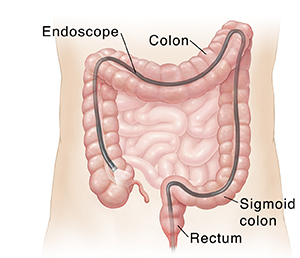 |
| Colonoscopy provides an inside view of the entire colon. |
After the test
You may have gas after the test. It can help to get rid of the gas to prevent bloating or discomfort. Your healthcare provider may talk with you about the results right away. Or you may need to schedule a follow-up visit to talk about the results.
You will need to have someone drive you home after the procedure.
You can go back to your normal eating and other activities after the test, if you are able to. You may be tired from the sedation and need to rest for the rest of the day. Ask your provider when you can take your regular medicines again. This is especially important if you are on any medicines that thin your blood. Some providers may want you to stop taking blood thinners for a few days after the test.
Restart your exercise program with walking when your provider says it's OK. Then slowly start to walk more if you are able to.
Drink plenty of water after your procedure. But stay away from any alcohol for 8 to 24 hours.
When to call your healthcare provider
Call your healthcare provider right away if you have any of these:
-
Severe belly (abdominal) pain
-
A bloated or firm belly
-
Fever of 100.4°F (38°C) or higher, or as advised by your provider
-
Rectal bleeding or bloody bowel movements
-
Nausea or vomiting
-
Weakness or dizziness
Online Medical Reviewer:
Marianne Fraser MSN RN
Online Medical Reviewer:
Melinda Murray Ratini DO
Online Medical Reviewer:
Robyn Zercher FNP
Date Last Reviewed:
3/1/2024
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.