A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
X
Y
Z
Click a letter to see a list of medical procedures beginning with that letter.
Click 'Back to Intro' to return to the beginning of this section.
When Your Child Has Mouth Sores
Your child has a mouth sore. These can be painful. They can make eating or drinking uncomfortable. But they are often not a serious problem. Most mouth sores can easily be managed and treated at home.
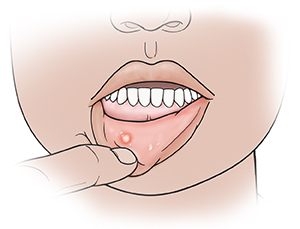 |
| A canker sore is a common mouth sore. It is often white and round in appearance. |
What are the symptoms of mouth sores?
Canker sores are the most common type of mouth sore. They are often white with red borders. Other types of mouth sores can be white, red, or yellow. Your child may have a single sore. Or they may have more than 1 at the same time. Mouth sore symptoms can include:
-
Pain
-
Swelling
-
Soreness
-
Redness
|
-
Drooling
-
Fever or headache
-
Being grouchy
|
Is it a mouth sore or a cold sore?
If your child has a sore outside the mouth, it’s likely a cold sore. Cold sores can be spread through direct contact. They may need different treatment than mouth sores. Ask your child’s healthcare provider for more information about cold sores if you think your child has one.
How are mouth sores diagnosed?
A mouth sore is diagnosed by how it looks. To get more information, the healthcare provider will ask about your child’s symptoms and health history. They will also examine your child. You will be told if any tests are needed.
How are mouth sores treated?
Mouth sores often go away in 7 to 14 days with no treatment.
You can do the following at home to ease your child’s symptoms:
-
Give your child over-the-counter (OTC) medicines, such as ibuprofen or acetaminophen, to treat pain and fever. Don't give ibuprofen to children age 6 months or younger. Don’t give aspirin to a child younger than age 19 unless directed by your child’s healthcare provider. Taking aspirin can put your child at risk for Reye syndrome. This is a rare but very serious disorder. It most often affects the brain and the liver.
-
Cold liquids, ice, or frozen juice bars may help soothe mouth pain. Don't give your child spicy or acidic foods.
-
Liquid antacid 4 times a day may help ease the pain. For children older than 6 years old, a teaspoon (5 mL) as a mouthwash may be given after meals. For younger children, put the antacid on the mouth sore using a cotton swab.
Use the following treatments only if your child is over the age of 4:
-
Put a small amount of OTC numbing gel on mouth sores to ease pain. The gel can cause a brief sting when used.
-
Have your child rinse their mouth with saltwater or with baking soda and warm water, then spit. The mouth rinse should not be swallowed.
When to call the healthcare provider
Call the healthcare provider if any of the following occur:
-
A mouth sore that doesn’t go away in 14 days
-
More mouth pain
-
Trouble swallowing
-
Signs of infection around a mouth sore (pus, drainage, or swelling)
-
Signs of dehydration (very dark or little urine, very thirsty, dry mouth, dizziness)
-
Fever (see "Fever and children" below)
-
Your child has had a seizure caused by the fever
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s healthcare provider may give you different numbers for your child. Follow your provider’s specific instructions.
Fever readings for a baby under 3 months old:
Fever readings for a child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.9°C) or higher
-
Armpit: 101°F (38.3°C) or higher
Call the healthcare provider in these cases:
-
Repeated temperature of 104°F (40°C) or higher in a child of any age
-
Fever of 100.4° F (38° C) or higher in baby younger than 3 months
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older
Online Medical Reviewer:
Amy Finke RN BSN
Online Medical Reviewer:
Heather M Trevino BSN RNC
Online Medical Reviewer:
Liora C Adler MD
Date Last Reviewed:
9/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.