A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
X
Y
Z
Click a letter to see a list of medical procedures beginning with that letter.
Click 'Back to Intro' to return to the beginning of this section.
Vocal Cord Dysfunction (VCD)
You have been told that you may have vocal cord dysfunction (VCD).
What is VCD?
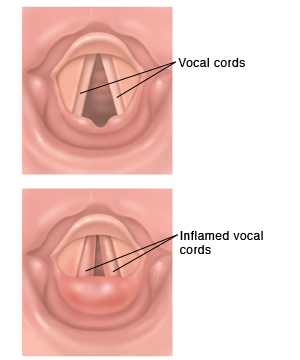
The vocal cords are 2 bands of muscle and connective tissue inside the larynx (voice box). The larynx rests at the top of your trachea (windpipe). This is in your throat. Normally, when a person breathes in and out, air flows through the vocal cords and in and out of the lungs, allowing the person to breathe easily. But with VCD, the vocal cords close when they should open. When you breathe in, instead of opening, the vocal cords close and cut off the air supply.
Sometimes another part of your voice box above or around the vocal cords is causing the blockage of your breathing. The problem is then called inspiratory laryngeal obstruction (ILO). VCD and ILO often have the same triggers and symptoms. They are also usually diagnosed and treated the same way.
What causes VCD?
The cause of VCD is often unclear. But these conditions or triggers can lead to it:
-
Post-nasal drip
-
Acid reflux, or gastroesophageal reflux disease (GERD)
-
Upper respiratory infections from a virus or bacteria
-
Exercise
-
Strong emotions, such as stress
-
Strong odors (fumes)
-
Cigarette smoke
Symptoms of VCD
Symptoms of VCD are like those for asthma. Sometimes people with VCD are thought to have asthma. But VCD symptoms are not eased by asthma medicines used to open the airway in your lungs, like bronchodilators. Also, symptoms of VCD often don't occur while you're sleeping.
Possible symptoms of VCD are:
-
Trouble breathing or shortness of breath. With VCD, you have more trouble breathing in than breathing out.
-
Noisy breathing (gasping, wheezing, or making raspy sounds)
-
Hoarseness
-
Voice changes
-
Repeated coughing or throat clearing
-
Tightness in the chest or throat
Diagnosing VCD
You may be asked to do breathing tests to measure how well air flows into and out of your lungs. Laryngoscopy may also be done. This test allows the healthcare provider to view your vocal cords using a thin, often flexible scope called a laryngoscope. Because symptoms of VCD are like those of asthma, tests for asthma may be done. Some people may have both asthma and VCD.
Treating VCD
The main treatment for VCD is learning to manage and control symptoms when they occur. Your healthcare provider may advise:
-
Speech therapy. This treatment teaches you how to control your vocal cords. A speech therapist or other specialist instructs you how to relax the muscles in your throat.
-
Relaxation techniques. Deep breathing, meditation, and activities like yoga can help reduce stress.
-
Biofeedback. This treatment teaches you how to control certain physical functions and responses. You learn how to reduce muscle tension.
-
Psychotherapy. This treatment involves working with a specially trained mental health professional about your problems. They can help you better cope with stress.
Other methods of treatment may be available. Your healthcare provider can tell you more, if needed.
Preventing VCD
To help prevent episodes of VCD, make changes in your life to reduce and manage triggers. If the cause of your VCD is a health problem such as acid reflux, you may need to take medicine and change certain eating habits. If you smoke, quitting can help you control VCD. Stay away from secondhand smoke, too. Don't let people smoke in your car or your home. Your healthcare provider can tell you more.
When to call 911
Call 911 right away if you have severe trouble breathing.
Online Medical Reviewer:
Ashutosh Kacker MD
Online Medical Reviewer:
Marianne Fraser MSN RN
Online Medical Reviewer:
Tara Novick BSN MSN
Date Last Reviewed:
7/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.