A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
X
Y
Z
Click a letter to see a list of conditions beginning with that letter.
Click 'Topic Index' to return to the index for the current topic.
Click 'Library Index' to return to the listing of all topics.
Having Catheter Ablation
A heart rhythm problem (arrhythmia) can make your heart beat too fast or in an irregular pattern. The problem is often caused by cells in your heart that aren’t working as they should. Or it may be due to an abnormal electric circuit. It may cause bothersome symptoms, such as an irregular heartbeat (palpitations), dizziness, shortness of breath, chest pain, or fainting. Your healthcare provider has advised catheter ablation to treat your arrhythmia. This nonsurgical procedure destroys the cells that are causing the problem.
Before the procedure
Before your catheter ablation, you'll meet with a specially trained heart healthcare provider (cardiac electrophysiologist) who will do the procedure. They'll tell you how to get ready. You'll likely be told to stop or change your heart rhythm medicines for a period of time before the procedure. Follow your provider’s instructions. Also:
-
Tell the healthcare provider about all prescription and over-the-counter medicines you take. This includes herbs, supplements, and vitamins. It also includes daily medicines, such as insulin or blood thinners. If you're allergic to any medicines, tell the provider.
-
Have any routine tests, such as blood tests, as advised.
-
Follow all directions you're given for not eating or drinking before your procedure.
How catheter ablation is done
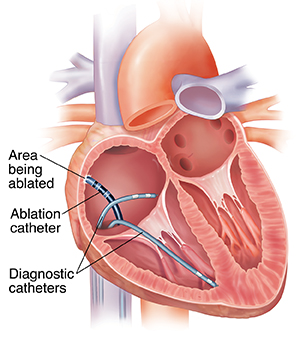
Catheter ablation uses thin, flexible wires (electrode catheters) to find and destroy (ablate) problem cells. Here’s how the procedure is done:
-
The heart’s signals are mapped. To find the problem, an electrophysiology study (EPS) is done. During this study, the healthcare provider records your normal heart electricity and then tries to start (induce) your arrhythmia. This is picked up by a diagnostic (mapping) catheter. An electrical map of the heart is then created. This shows the type of arrhythmia you have and where the problem is. Using the map as a guide, the provider knows where to ablate.
-
Problem areas are destroyed using heat or cold therapy. Once the EPS shows where the problem is, the provider threads an electrode catheter through a blood vessel to that area in the heart. Energy is sent through the catheter to destroy the problem cells.
-
The heart’s rhythm is tested again. After ablating the problem cells, the provider tries to restart (reinduce) your arrhythmia. If a fast rhythm can’t be induced, the ablation is a success. But if a fast rhythm does start again, you may need more ablation.
Your experience during catheter ablation
In most cases, catheter ablation is done in an electrophysiology lab. It often takes 2 to 4 hours, and sometimes longer. You’ll receive medicine to prevent pain. Medicine will also help you relax or sleep during the procedure. If you feel uncomfortable during the procedure, tell the healthcare provider or nurse. In some cases, you may have general anesthesia.
-
First, the healthcare team washes the skin on your groin (or rarely, the neck). Any hair in that area may be removed. This is where the catheters will be inserted. An IV (intravenous) line is started in your arm. Medicines and fluids are given through this IV. To help keep the insertion site germ-free (sterile), your body is draped with sheets. Only the area where the catheters will be inserted is exposed.
-
The healthcare provider numbs the skin where the catheters will be inserted with pain medicine (local anesthetic). Then the provider uses a small needle to make holes (punctures) in your vein or artery. They put catheters through these punctures and guide them to your heart. The provider may use X-ray monitors or other mapping or navigation systems to help guide the catheters.
-
The provider then puts wires in several places in the heart to map the electrical signals. The wires also stimulate the heart.
-
When the procedure is done, the provider takes the catheters out of your body. They put pressure on the puncture sites to stop any bleeding. Sometimes the provides uses a vascular access closure device to stop the bleeding. You’re then taken to a recovery room to rest. You'll need to remain lying down for 2 to 6 hours. You'll also be asked not to move the leg where the catheters were inserted for a few hours. This is to make sure the insertion sites don't bleed. For many procedures, you may be able to go home on the same day as the procedure.
Risks and possible complications
The risks of catheter ablation are fairly low compared to the benefits you receive. Discuss these risks with your healthcare provider before the procedure. Possible risks and complications include:
-
Bleeding or bruising at the catheter insertion site
-
Blood clots
-
A slow heart rhythm (requiring a permanent pacemaker)
-
Small hole (perforation) in the heart muscle, blood vessel, or lung (may need an emergency procedure)
-
Damage to a heart valve (rare)
-
Stroke
-
Heart attack, also known as acute myocardial infarction, or AMI (rare)
-
Infection, which is a risk after any invasive procedure. This may be indicated by a fever of 100.4°F (38°C) or higher, fluid leaking, or redness and pain at the catheter insertion site.
-
Death (extremely rare)
Online Medical Reviewer:
Ronald Karlin MD
Online Medical Reviewer:
Stacey Wojcik MBA BSN RN
Online Medical Reviewer:
Steven Kang MD
Date Last Reviewed:
3/1/2024
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.