A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
X
Y
Z
Click a letter to see a list of medical procedures beginning with that letter.
Click 'Back to Intro' to return to the beginning of this section.
When Your Child Has Pleural Effusion
The area between the chest wall and lung is called the pleural space. The lining around this space produces small amounts of fluid. This fluid helps lubricate the lining and allows the lungs to expand smoothly. Pleural effusion occurs when too much fluid builds up in the pleural space.
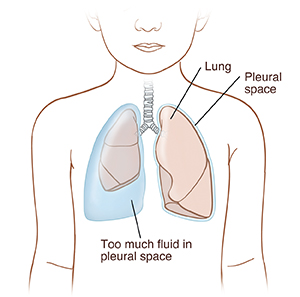 |
| Fluid buildup in the pleural space can compress the lung and cause problems with breathing. |
What causes pleural effusion?
Pleural effusion can occur if your child has a lung inflammation or infection. It can also happen if fluid builds up after surgery. Sometimes a pleural effusion may be caused by problems in the heart, kidney or liver. It can also be caused by an injury or other inflammatory diseases. If not treated, pleural effusion can lead to serious breathing problems. That’s why your child needs treatment right away.
What are the symptoms of pleural effusion?
Pleural effusion may not cause symptoms. If symptoms occur, they can include:
How is pleural effusion diagnosed?
Your child’s healthcare provider listens with a stethoscope and taps on the chest. One or more of the following tests may be done to confirm the diagnosis:
-
Chest X-rays. These are taken in different positions to check if air or fluid is in the pleural spaces.
-
Ultrasound or CT scan. These are done if a chest X-ray does not give a clear picture. These tests may give a better picture of locations and pockets of fluid in the pleural space.
-
Pleural fluid analysis. A needle is passed into the pleural space to remove fluid. The fluid is then sent to a lab for testing.
How is pleural effusion treated?
Treatment depends on how much fluid is present and if it is infected.
-
If there is a small amount of fluid, it will likely go away on its own. The healthcare provider will have you watch your child at home. No hospital stay is needed.
-
If your child has a lot of fluid or pus, is having trouble breathing, or is uncomfortable, they may need to stay in the hospital. They may have a thoracentesis. This is when a needle is put into the pleural space to remove extra fluid. Or, they may have a chest tube placed to drain the fluid.
-
If your child has an infection, antibiotics may be given to treat it.
-
The healthcare provider will identify and treat any other underlying problem.
What are the long-term concerns?
Often, the causes of pleural effusion in children are less serious than for adults. Your child should have no long-term effects once the underlying problem is treated. The healthcare provider can tell you more about your child’s condition and what to expect.
When to call your child's healthcare provider
Unless advised otherwise by your child’s healthcare provider, call the provider right away if any of these occur:
-
Trouble breathing
-
Rapid breathing
-
Coughing up blood
-
Chest pain that continues or gets worse
-
Fever of 100.4° F ( 38.0°C ) or higher, or as directed by your child's provider
-
Other symptoms get worse or new symptoms appear
Online Medical Reviewer:
Jessica Gotwals BSN MPH
Online Medical Reviewer:
Liora C Adler MD
Online Medical Reviewer:
Marianne Fraser MSN RN
Date Last Reviewed:
6/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.