Having Posterior Tibialis Tendon Surgery
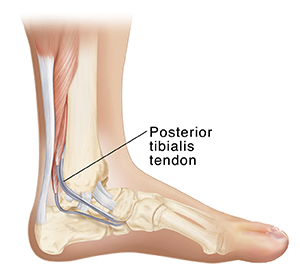
Posterior tibialis tendon surgery is a way to fix the tendon on the back of your calf that goes down the inside part of your ankle. The tendon can be torn or inflamed from injury or other causes. This can cause pain and other problems. Surgery can help relieve these problems.
What to tell your healthcare provider
Tell your healthcare provider about all the medicines you take. This includes over-the-counter medicines such as ibuprofen. It also includes vitamins, herbs, and other supplements. And tell your healthcare provider if you:
-
Have had any recent changes in your health, such as an infection or fever
-
Are sensitive or allergic to any medicines, latex, tape, or anesthesia (local and general)
-
Are pregnant or think you may be pregnant
Tests before your surgery
Before your surgery, you may need imaging tests. These may include X-rays and MRI.
Getting ready for your surgery
Your surgery will be done by an orthopedic surgeon. This is a surgeon who specializes in treating bone, muscle, joint, and tendon problems. Talk with your surgeon about how to get ready for your surgery. You may need to stop taking some medicines before the procedure, such as blood thinners and aspirin. If you smoke, you may need to stop before your surgery. Smoking can delay healing. Talk with your surgeon if you need help to stop smoking.
Also, make sure to:
-
Ask a family member or friend to take you home from the hospital
-
Follow any directions you are given for not eating or drinking before surgery
-
Follow all other instructions from your surgeon
You will be asked to sign a consent form that gives your permission to do the procedure. Read the form carefully. Ask questions if something is not clear.
Planning your recovery
You will also need to plan some changes at home to help you recover. You may need help at home. You may need to plan changes to your activities. You won’t be able to walk on your foot normally for a while.
On the day of your surgery
Your orthopedic surgeon will work with a team of specialized nurses. The surgery can be done in several ways. Ask your surgeon about the details of your surgery. The procedure may take a couple of hours. In general, you can expect the following:
-
You may have spinal anesthesia, so you won’t feel anything from the waist down. You will also be given medicine (sedation) so you’ll sleep through the surgery. Or you may have general anesthesia to make you unconscious during the surgery.
-
A healthcare provider will watch your heart rate, blood pressure, and other vital signs.
-
The surgeon will make a cut (incision) through the skin and muscle of your lower calf.
-
If you are having minimally invasive surgery, the surgeon will make a small incision. They will then use small tools and a tiny camera to do the surgery.
-
The surgeon will make an incision through the sheath that surrounds the tendon. They will then remove or repair parts of your damaged tendon.
-
The surgeon may remove another tendon from your foot. This is then used to replace part or all of your posterior tibialis tendon.
-
The surgeon will close the layers of skin and muscle around your calf with stitches (sutures), staples, or other means.
After your surgery
After the procedure, you will spend several hours in a recovery room. You may be sleepy and confused when you wake up. Your healthcare team will watch your vital signs, such as your heart rate and breathing. You’ll be given pain medicine if you need it. Your ankle will be in a splint. You may be able to go home the same day. Or you may stay overnight in the hospital.
Recovering at home
Follow all of your healthcare provider's instructions about pain medicines and wound care. You will have some pain after your surgery. Medicines can help lessen your pain. Keep your leg raised when you sit down. Do this as often as possible. This can help reduce swelling and pain. You’ll need to use crutches and keep your weight off your leg for several weeks.
Follow-up care
Your stitches or staples may be removed about 10 to 14 days after surgery. Your splint may be replaced with a cast at this time. Follow all instructions about keeping your cast dry. Or you may be given a removable boot instead of a cast.
Your surgeon will give you instructions about when you can put weight on your leg and how to strengthen your ankle and leg muscles as you recover. You may need to do physical therapy. You may have pain for months before you start to notice major benefits from your surgery. Follow all of your surgeon’s instructions about postsurgery exercises. This will help to make sure the surgery is a success for you.
When to call your healthcare provider
Call your healthcare provider right away if you have any of these:
-
Fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider
-
Shaking chills
-
Pain in your ankle or calf that gets worse
-
Boot or cast that seems too tight or too loose
-
Cast that gets wet or soggy
-
Pale color or other change in color of the skin around the cast
-
Numbness or tingling near or under the cast or to the foot
-
Toes that are numb or turn blue or pale
-
Redness, swelling, warmth, bad smell, or fluid at the incision site